Are you getting heel pain when running? Or in the first few steps out of bed in the morning? If so then you may be suffering from the dreaded Plantar Fasciitis. Plantar Fasciitis is the most common cause of heel pain when running. In this article, we’re going to take a deep dive into the plantar fasciitis beast. We’ll talk about what it it and why you got it. We’ll review some of the latest research on the subject in order to get you the most up to date information. Then in part two we’ll look at your treatment options.
What is Plantar Fasciitis?
So what exactly are we talking about here? The plantar fascia is a band of connective tissue that supports the arch of the foot. From the heel bone (calcaneus) it fans out and inserts into all the toes (metatarsal heads). The plantar fascia is made of the connective tissue collagen. This is similar to the collagen we have in our ligaments and tendons.

The most common cause of heel pain when running is Plantar Fasciitis. Plantar Fasciitis is a term commonly used to describe pain in the heel on the underside of the foot. Sometimes the pain extends further into the arch of the foot but often it’s quite localised to the heel.

Back in the day we believed that the plantar fascia was being mechanically overloaded resulting in microtears and chronic inflammation of the plantar fascia. With a bit more study into what is actually happening on a cellular level this does not appear to be quite right. It seems more like a degenerative type problem as opposed to an acute inflammation (Lemont 2003). Since ‘-itis’ literally means ‘inflammation’ we can’t really call it plantar fasci-itis anymore. For this reason it’s a bit more trendy to call the problem Plantar Fasciopathy and, since I’m a trendy dude, that’s what I’ll be calling it. This is very similar to the change from tendontis to tendinopathy.
Actually, many clinicians are using the term “plantar-heel-pain” nowadays but I just can’t bring myself to tell my clients they have “sole-of-heel-pain” because they already know that!
Do I have Plantar Fasciitis?
Plantar fasciitis fasciopathy is a clinical diagnosis. So a Physiotherapist, Athletic Therapist or Sports Physician can diagnose the problem with a clinical examination. It also means that you do not require imaging such as MRI scans or ultrasound scans to make the diagnosis.
To diagnose heel plantar fasciopathy in the clinic here are the signs and symptoms that I will look for:
- Pain localised to a small area on the inside of the sole of the heel that is tender when you press on it (medial calcaneal tubercle)
- Heel pain with the first few steps out of bed in the morning
- Heel pain when running, walking or standing for prolonged periods
There are some other conditions that can give you heel pain when running, however, if you have the symptoms described above there is an extremely good chance you have plantar fasciopathy. Here are some of the alternative causes:
- Tarsal Tunnel Syndrome – usually you will also have tingling or numbness in the foot
- Retrocalcaneal Bursitis – pain is on the back of the heel, not the sole
- Insertional Achilles Tendinopathy – pain is on the back of the heel, not the sole
- Stress Fracture of the heel bone (calcaneus) – hard to diagnose, you may need the help of a clinician
- Fat Pad Atrophy – another one that is hard to diagnose, again you will need the help of a clinician

Why do I get Heel Pain when Running?
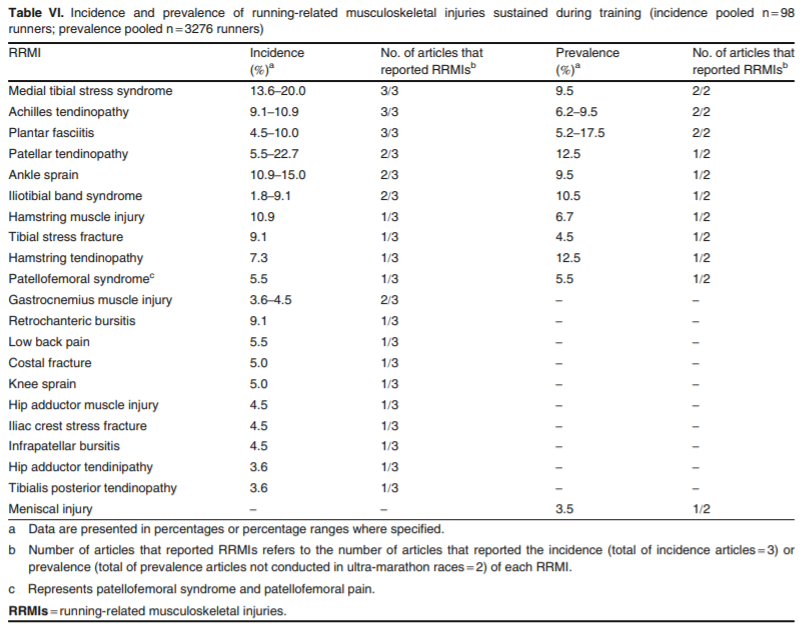
Plantar fasciopathy is the most common cause of heel pain when running. In fact, it is one of the top 5 running injuries with an incidence of 4.5-10% (Lopes 2012). That means if you go to the running club this week and there are 10 people running, 1-2 of them will get plantar fasciopathy within the year.
There are some other things that make you more likely to get plantar fasciopathy. We call these Risk Factors. Some are non-modifiable like being female or being aged 40-60. Some are modifiable which means we can potentially do something about them.
Modifiable Risk Factors for Plantar Fasciopathy
- High impact during running
- Stiff ankle / tight calf
- BMI >25 kg/m²
- Flatter foot arches in standing position (increased pronation)
- Spending most of the work day on your feet, especially on hard surfaces
- Wearing the same shoes every day
Monteagudo 2018, Werner 2010, Pohl 2009, Riddle 2003
High Impact During Running
I’ve talked a lot in the past about how reducing impact is important for preventing running injuries. In their 2009 study Pohl and colleagues found that runners who already had plantar fasciopathy tended to land with more impact. Essentially this just means that they hit the ground harder on each stride. The fancy term for high impact is high Vertical Loading Rate which has been associated with the development of other running injuries (Davis 2016).
So if landing with more impact per stride puts you more at risk of developing plantar fasciopathy, it’s probably a good idea to run with less impact. To do that you’ll need to learn to run more softly – check out my article here.
A word of caution on this one. High impact was only associated with runners who already have plantar fasciopathy and it was only identified in this one study (Pohl 2009). Running softly is probably a good idea overall but it doesn’t mean you definitely wont get plantar fasciopathy.
Stiff Ankle / Tight Calf
This risk factor is more well established and well worth some time to address in my opinion. What we are most concerned with is your range of movement in pulling the foot up towards your face (dorsiflexion). If you have a look at the images below you can see the range of dorsiflexion measured with the knee straight and with it bent.
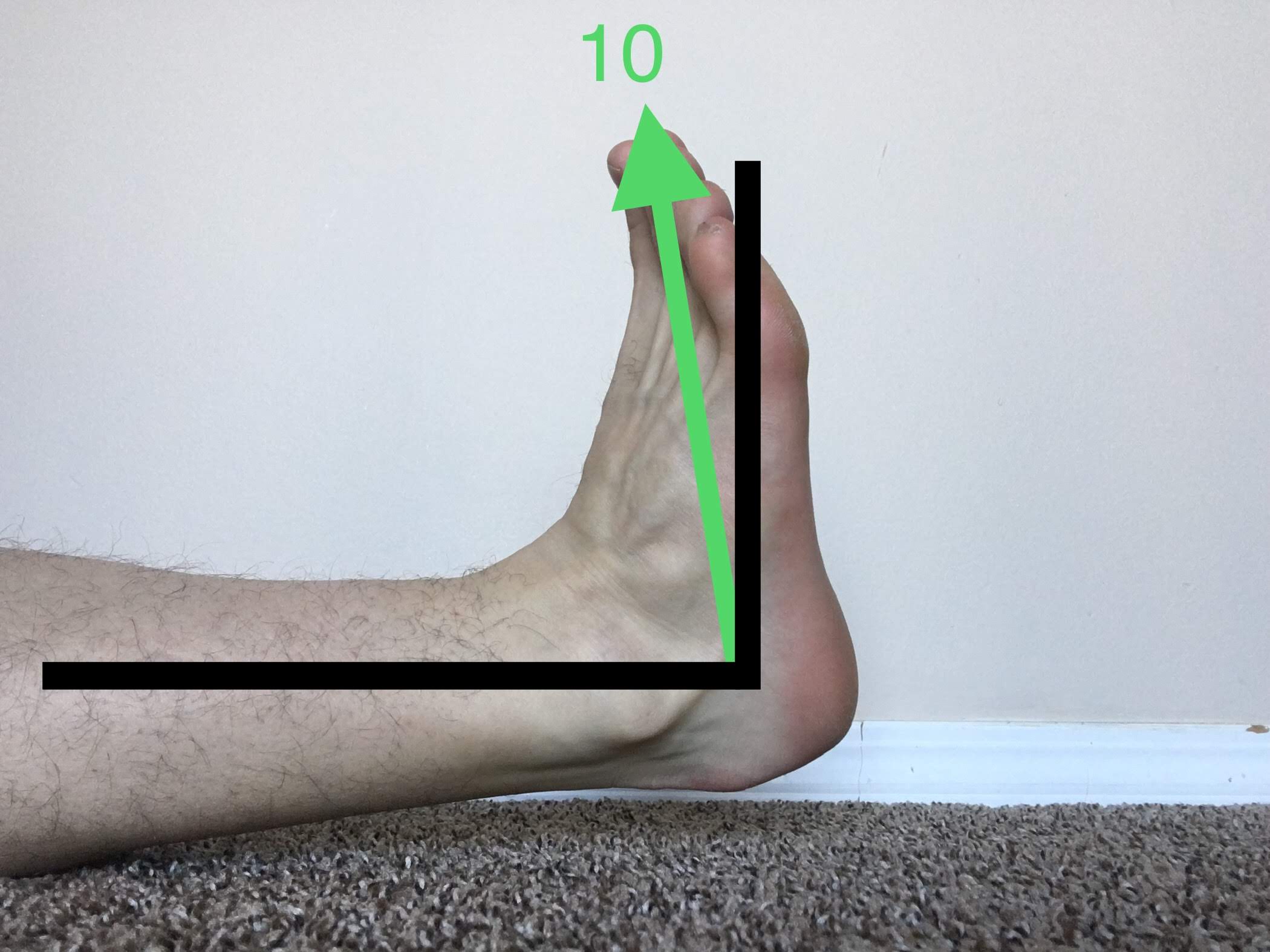

We want to measure range of movement with the knee bent and with it straight to check that we have enough flexibility in both parts of our calf muscle (the gastrocnemius and the soleus). If you have less than 10° dorsiflexion with the knee straight or less than 10cm on your knee to wall test then you need to improve your flexibility.
The best way to do this in my opinion is not actually through stretching but rather through strengthening. We’re going to talk more about that in part two of this blog on plantar fasciopathy treatment so stay tuned for that.
BMI >25 kg/m²
Unfortunately a high BMI has been consistently shown to be associated with a higher risk of developing plantar fasciopathy. Individuals with a BMI of > 25kg/m² have a two-fold risk of developing plantar fasciopathy and those with a BMI > 30kg/m² have a five-fold risk (Riddle 2003)
This can be incredibly frustrating as many people use running as a way to help them manage their weight. Dietary advice is definitely outside of my scope so I’m afraid I can’t offer much assistance on this front. However, I do have some suggestions for those with a higher BMI who are looking to increase their running.
Basically, if you have a higher BMI then you are more at risk of developing an injury. That means it’s even more important that you manage your training load really carefully, progress really slowly, work on your running technique and incorporate some strength training. If you already have plantar fasciopathy but want to keep training then I suggest you read up on cross training for injured runners.
Flatter Foot Arches in the Standing Position
Here is where we start to delve into the muddy water of orthotics. I’m going to talk more about that in part two of this series on treatment so I’m going to leave this one alone for now.
Spending Most of the Work Day on Your Feet, Especially on Hard Surfaces
As a runner you might not think this applies to you so much. However, time on feet during the day has been consistently shown to be a risk factor for developing plantar fasciopathy. The most difficult cases of plantar fasciopathy I see in the clinic tend be in people who can’t avoid standing and walking at work. This includes manual labourers, police, factory workers, retail workers etc.
If you do have one of these jobs it’s a bit of a double edged sword. Your heart, lungs, blood vessels and all that other good stuff will really benefit from all that free exercise. Your poor heels might get sore though! Some institutions have brought in cushioned floors and encourage people to wear cushioned shoes/boots. I’m not sure how well these interventions work but I would suggest scheduling regular breaks if you spend all day on your feet. Just a 2-5 minute sit down once every hour or two should be enough. Please bear in mind that I have no evidence for this particular recommendation!
Wearing the Same Shoes Every Day
I’ve written previously about how rotating through more than one pair of running shoes during the week can have a protective effect against injuries. Just have 1-2 pairs of running shoes and switch from one to the other each run. I’d suggest making the shoes a different brand or at least a different model.
I know this is sacrilege to some runners who take their shoe fidelity as seriously as their marriage vows. However, it’s important to remember that almost all running injuries are repetitive stress injuries (overuse injuries). Switching shoes will put the stress on different parts of the foot and reduce the risk of overloading the plantar fascia.
Heel Pain when Running – Conclusions
Now we know what plantar fasciopathy is and we’ve talked about some of the reasons you might have developed it. We’ve also talked about some ways to try to prevent it by studying the research on the risk factors. In Part Two of this article, we’ll dig into the different treatment options and try to make sense of them all. Part Two: